
Surprise flowers sent with love from Jen
I felt great Tuesday and had a busy day at work followed by a really strong workout at the gym then took the girls out for a walk to let them enjoy the spring weather. After finally settling back into the house and eating dinner, I had to call the hemonc fellow on-call for magic mouthwash (a prescription mouthwash containing lidocaine) because my mouth sores had worsened and I found myself avoiding eating because of the pain. During the half hour Jason was gone to pick up the mouthwash, I took a turn for the worst and started feeling horrible with chills, body aches, and a headache. I fell asleep with the girls for a few hours and woke up around midnight with a fever of 100.3. While going through chemotherapy, I have to watch for fevers of 100.5 or greater, and at that point, I have to go to the emergency department (ED). My fever ranged from 99-100.4 throughout the rest of Tuesday night and Wednesday. Around 3:30pm Wednesday, I started to have readings of 100.5, but not consistently, so I monitored my temperature about every 10-15 minutes, and was staying just under 100.5. Jason and I had planned to stay at the Carolina Inn on Wednesday night before the PET and CT scans on Thursday, so we could go over and enjoy trying a new restaurant and relax before the scans. As we were about 15 minutes from the hotel around 6:40pm, I felt my temperature spiking, so I checked it and it was up to 101. As we finished our drive to the hotel, I checked it every five minutes and kept getting reads around 101-101.5, which we knew meant we had to go straight to the ED. We checked in quickly, and I packed some lounge clothes, essential toiletries, and my computer and iPad in anticipation of being kept at the hospital.
My 4-Onc “welcome package”
I got checked into the ED at UNC Chapel Hill and was immediately given a mask, and only had to wait about 15 minutes before being taken back to to a private room. There is a strict protocol for diagnosing cancer patients currently undergoing chemotherapy when they have fevers. The nurse accessed my port, which had not been numbed, and she had a difficult time getting the needle to lock in place, pushing and readjusting several times, which was extremely painful. She was finally able to do several cultures to check for infection in my port and draw blood to check my blood levels and for other signs of infection. They also swabbed my nose to check for the flu and required a urine sample. All of these samples were sent off to the lab, and the oncologist reviewed them once the tests were complete. By 10pm, the oncology team had reviewed my labs and decided they would be admitting me. I was transported up to the inpatient oncology unit and relieved to be put into a nicely sized private room and private bathroom, and more importantly away from the crazy germy people in the ED. I was finally settled into my room around 10:30, and Jason went out to pick us up dinner from one of the Franklin Street bars. After eating dinner, my nurse started me on strong antibiotics through the IV (vancomycin and cefepime). Throughout the rest of Wednesday night, my nurse Driss had to come into my room about once an hour to either check vitals, change my IV bags, or give me heparin shots (used to prevent blood clots). I only slept at most four hours because of all of this and by 7am Wednesday, the inpatient oncology team was doing rounds and came in to see me.
My inpatient oncology team is made up of an attending, resident, intern, med student, pharmacist, and nurses. At this point, I was told that I would have to go 48 hours without having a fever before I could be released, and that they wanted to see my counts rise. This crushed my thoughts that I would come in get some antibiotics and be sent home, which were based purely on my speculation of how this process worked. Dr. Muss, Dr. Lincoln, and Johann all came back in a few minutes later and discussed the plan to treat me with broad spectrum antibiotics to kill anything that could be in my system, although all of my cultures were negative. They noted that my blood counts were low, and that since I was exhibiting no other symptoms besides the fever, it was likely a neutropenic fever, which is a result of my blood counts starting to rise, so they would continue to monitor me and my cultures and thought it should only be a couple of days until my counts rebounded and the fevers should stop. After meeting with my team, I was taken down for my PET and CT scan, which took about three hours and went smoothly. After I was done, the transport team sent someone to take me back up to my room on the fourth floor. However, as he was wheeling my hospital bed along, I noticed we were going down the hallway toward the ED, and found my observation to be correct very shortly thereafter. He parked my bed and left me in the ED hallway, and said he’d be right back. I immediately started to freak out, because I knew I should not be in the ED since being exposed to the number of germs and bacteria roaming through the ED hallways was extremely dangerous to me with as a cancer patient with very low blood counts. I flagged down the first nurse I saw and requested a mask and told her with a panicked sound in my voice that I was a cancer patient admitted to 4 onc and that I was not supposed to be there and needed to be taken upstairs immediately. She gave me a mask and said she’d tell the transport team and they would get me taken back up.
As I sat in this hallway, the first patient that was wheeled by me had eyes that were as yellow as Gerber daisies, which caused mine to become the size of saucers and set off a higher wave of panic. Fortunately, I had taken my phone with me to my PET as entertainment for the hour long waiting period while I waited for the contrast infusion and started texting Jason to alert him to the situation. He told my nurse Christie who confirmed that I should absolutely not be in the ED and to start yelling at any and every doctor or nurse that I saw to take me back up to the fourth floor. I made many fruitless attempts to get hospital staff members’ attention between texting Jason who was standing with Christy, I watched countless sick patients at best be wheeled past me, or at worst be parked beside me, and cringed and snarled at each one fearing that every one of them had Ebola. After 50 minutes of this pattern, I finally got the attention of one nurse who assured me she would be sure I was taken back upstairs. After terrifying and angering hour of sitting in the ER hallway, the aforementioned nurse brought a transporter over to me, and he took me back up to the onc unit. At the same time Patrick was getting me wheeled around, some of Christy’s calls had made their way over to the radiology unit in addition to the ED, and Jeanie (who was one of the radiology technicians that had just completed my PET/CT scans) came walking up to me ready to wheel me upstairs herself if necessary. She told me that she had just figured out the original transporter had an old list from Wednesday night before I had been admitted to 4 Onc, and that was the cause of the whole mix up that landed me in the ED hallway for an hour. I never saw the original transporter again after he dropped me off in the ER hallway, so what happened to him is a mystery to me. Once back upstairs, I was greeted by Jason and Christy who were as relieved to see me as I was them. Christy, who is very sweet, energetic, and protective, was as riled up as I was about the whole situation, and let me know she filed a complaint with the transport department and that they should know better than to put a patient like me at such risk. I was relieved to know that I had not been overreacting due to the fact that I had not eaten since 11pm the night before, and also to be safely back in my protected unit.
The rest of Thursday went much more smoothly, although I was still fighting a fever around 38-38.5C, I was able to walk around the onc unit and got an off unit pass to go down to the atrium. I laughed at the necessity of getting a pass from the nurses and wearing this large green sticker on my shirt, but was so thankful to feel sunshine, breathe fresh air, and not feel like a complete prisoner. When I came back from my time outside, Dr. Lincoln skipped into my room excited to tell me that she had done a preliminary read on the PET scan and although her ability to read PETs is somewhat rudimentary, it showed that I had no new growth, I had strong shrinkage in the affected nodes, and that it was consistent with a good response to chemotherapy. She said she was very pleased with the results and wanted to pass the good news along before leaving for the night. I was thrilled to hear this, although I knew we would still have to wait on the clinical trial doctor’s and Dr. Park’s read of the scans.
My fevers started to increase early Thursday evening again and throughout the night. I was awoken every couple of hours for blood work, shots, and medicine changes again, which resulted in another night of about 4 hours of sleep. When I woke up Friday, Johann (the intern) was the first from the team to come see me, and let me know that because I had fevers over night, it restarted the 48 hour clock, which meant I couldn’t be released at least until Saturday. I felt an overwhelming number of emotions upon hearing this news, which Jason could apparently see written all over my face. He reassured me that the doctors were taking good care of me and ensuring I was healthy and able to continue with my treatment and empathized with my frustration of being stuck in the hospital with no way of knowing when I would be released and with being scared of these high fevers and potential infections. After a few minutes of talking and hugs, I went to take a shower and dance out my emotions, because I refused to succumb to negative emotions and cry for the first time since shaving my head. After blasting some Wyclef, Rihanna, and Jay-Z, I came out of the shower feeling renewed and empowered and ready to take on the day. I went through Friday with my fever staying just below the technical fever threshold and felt good, walking laps around 4-Onc and getting another unit pass to go out to the atrium, all the while hoping this was the start to the countdown to my release. Friday night, after Jason and I had dinner and started watching House of Cards, I felt myself feeling febrile. I tried drinking ice water in an effort to ward off a fever. Unfortunately, around 9pm after about 2 hours of fighting it, it reached a point where I checked my temperature and was getting a read of over 39C, so we decided to alert my nurse Rheagan. She checked my temperature and confirmed it was a high fever that required immediate action. She went off to consult with the oncologist. While she was gone, I completely lost it and was unable to dance it off. I cried and expressed to Jason every fear and thought going through my head from the fact that this was a sign that the chemotherapy wasn’t really working to the fear that something was seriously wrong and that I could take a quick turn for the worst and that they couldn’t help me.
I washed my face and pulled myself together, feeling better after verbalizing my emotions. The oncologist ordered regular blood work, a chest scan, and blood work done by the phlebotomist. Rheagan came running back in the room to pull the blood work quickly, because the radiology technician was walking down the hallway with the portable x-ray machine. As soon as they were both done, the phlebotomist was in my room drawing blood from my arm for cultures. After he was done, I called my brother who reiterated that I was in the right place for having a fever and that they were following all standard precautions, performing the proper tests, and putting more thought into me than I am aware. That helped me to relax and be able to get to sleep shortly thereafter, at least until I woke up with a fever again. Rheagan was fantastic in her care of me and was able to change my IV medications without waking me and only had to wake me for the two vitals checks. I woke up around 3:30am with another high fever, headache, and feeling dizzy. I finally woke up around 9am Saturday, feeling more rested than I had on the four hours or so of sleep I had gotten Tuesday through Thursday nights. I took it easy Saturday morning, eating breakfast and reading the paper while waiting for my team to come in for a visit. Once they came in, we discussed the excitement of the fevers and testing from the night before. They noted all of the original and new cultures were clear and my chest x-ray looked perfect, which ruled out all bacterial and viral infections they could think of without going into really far fetched possibilities, which didn’t seem realistic given my lack of other symptoms. We decided to continue course with the broad spectrum coverage of the vancomycin and cefepime and monitoring, hoping that my blood counts would start to rise on their own. They noted again that they were surprised that we had not seen any increase in my counts and decrease in my fever since I had been admitted, but hoped that it was just a case of slow response and that I would start to respond over the course of Saturday.

My IV pole with infusion machines and paper origami crane mobile made by hospital volunteers for luck and wellness. (Also notice the white board in the back where they keep a list of all of my staff from doctors to nurses to houskeeper, and latest test results)
Saturday took a turn for the worst after lunch. I had planned to go out for my walks and get outside for fresh air, but after lunch was unable to do anything but nap. I woke up after my first hour of napping and instead of feeling refreshed like I hoped, I felt greatly fatigued and febrile. I decided to try to sleep it off, and continued this pattern over the next four hours. By 4:00 my fever reached 39.8C. My nurse Emily got Dr. Lincoln to come and do an exam because of this very high fever. Again, Dr. Lincoln examined me and search for any possible explanation for this fever, but couldn’t find any. She told me that a fever this high really scares doctors and that she and the other doctors on my team were quite perplexed as to why my counts were continuing to sit so low and my fever persisting, and that they were frustrated and wanted to see me recovery quickly since I look so good and have done so well otherwise. She decided to broaden the coverage of the antibiotics and change the cefepime to meropenem, which is stronger and broader and covers gut bacteria, and keep me on the vancomycin. Without indication of any causes, she gave me some Tylenol to lower my fever, and within 45 minutes it was back down to 37.8.
I made it through Saturday night without a fever. Sunday morning, I discussed the 39.8C fever with Dr. Muss and, he like Dr. Lincoln, was without real explanation or understanding of how quickly and high it came and went. In a last ditch effort to cover all bases, after discussing some international travel I had done in the past several years, Dr. Muss decided to order labs to check me for parasites and C. Diff, which meant I wasn’t allowed to leave my room and if I did I had to wear a yellow suit and gloves, so I spent all of Sunday locked in my room until that was ruled out. Finally, by 5pm, and just before sunset, C. Diff was ruled out, and I was allowed to leave my room. I was also surprised by Daniel showing up after driving seven hours to come be with me. After visiting for a few minutes, Jason and Daniel decided to walk and go get us non-hospital food for dinner, so I took that time to take the paper and my phone and go sit outside and listen to music and read. It was such a tremendous few minutes to sit outside watching the American flag wave in the breeze and feeling warmth of the setting sun. I felt peaceful and finally relief knowing I had made it to being fever free for almost 24 hours.
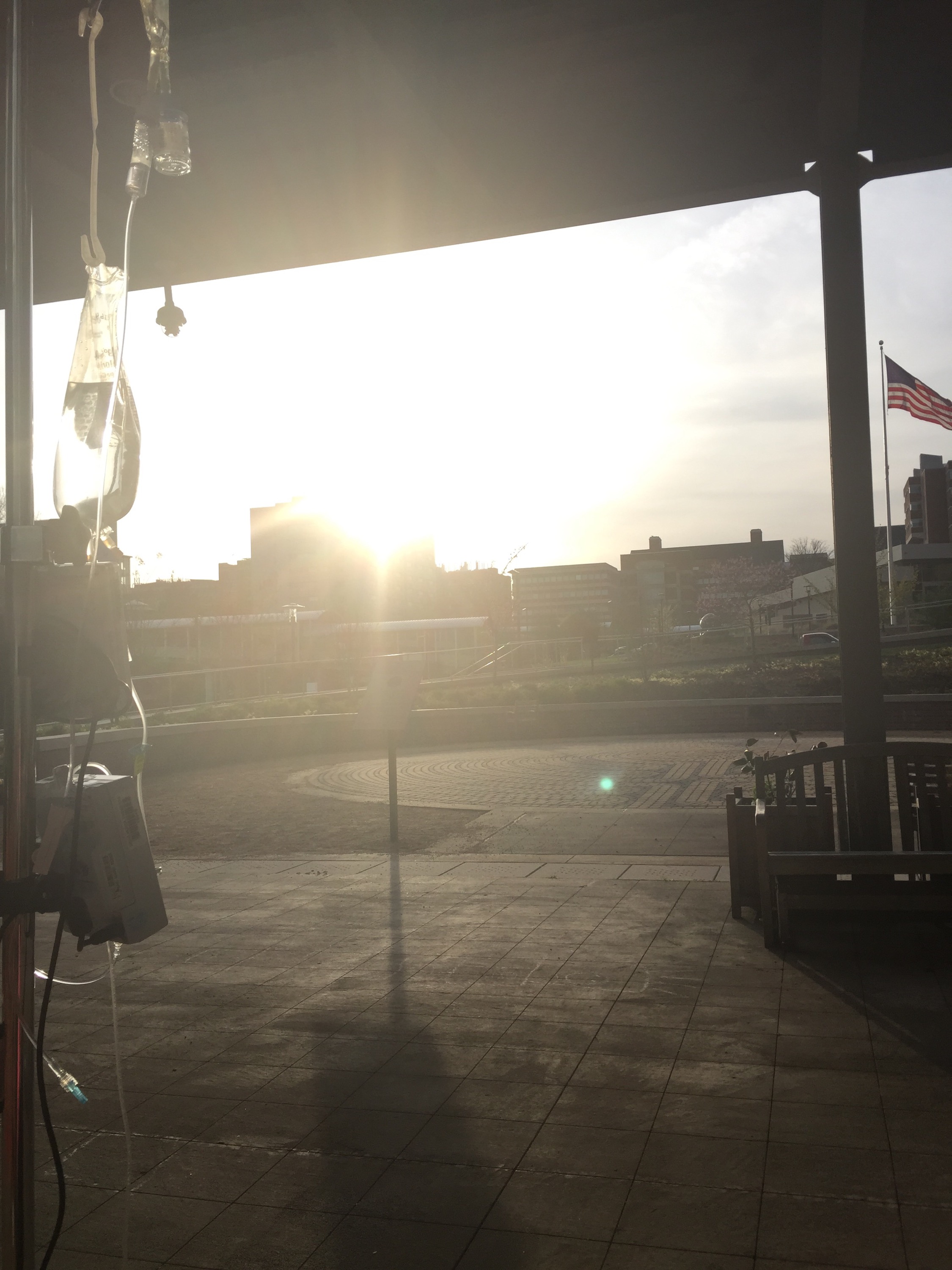
View of freedom and breath of fresh air after two days of barely leaving my room.
I made it through the night again last night sleeping relatively well with minimal and quiet interruptions by my night nurse Julia, and most importantly, without the need for additional tests and x-rays or fevers. When meeting with my team this morning, they were happy to report that all of my blood counts beside my ANC (absolute neutrophil count-a type of white blood cell) showed a nice bump from Saturday midnight counts to Sunday midnight counts. My ANC is still sitting at 0.5, which they noted is still on the cusp of being neutropenic (below 0.5), but that it is the last to rise and normally follows after the others rise. They are likely going to keep me overnight tonight even though I should hit the 48 hour fever free mark around 6pm tonight just to be able to monitor my blood counts a little longer and hopefully see the ANC rise. They are consulting with Dr. Park today as well to discuss whether my chemotherapy tomorrow will need to be delayed due to my counts, and whether we will do a quick acting stimulation to increase my counts. Hopefully, they will come back this afternoon with good news from Dr. Park, and I will have a planned end to my hospital stay.
Although I am five nights and counting into my hospitalization, I am seriously impressed with the genuineness, compassion, and quality of care the doctors and nurses have provided. They have commented on my optimism and energy, and I think they have greatly contributed to mine. I am also immensely thankful Jason has been here to sit with me, keep me company, bring me non-hospital food and clean clothes, anxiously watch the vitals machine as it beeps and produces current reads on my levels, and be the one to remind me that I am strong and can get through this. My family has been my rock through this and FaceTimed and texted constantly keeping me focused and holding me up when I couldn’t do it myself. I have had friends calling, emailing, texting, and sending flowers, making me feel loved and making me laugh. The stress of this hospital stay was probably made worse with the wait for the results tomorrow, but in all, with only one breakdown, I have been accepting of this as part of the journey and trusting in the doctors’ knowledge, skill, and care. (not to say I want to be a permanent resident of 4-Onc…I miss Annabelle and Layla terribly)

Jason testing out his new bed
I am so happy to hear that you’re fever free! I hope you’re at home or getting to go home today, and I hope that you get tons of kisses and cuddles from your sweet girls!!!! You’re in my thoughts and prayers sweet girl!
I want to say thanks 4 creating this site and keep going the great job!